Postural concept
What is the posturo-occlusal concept?
The posturo-occlusal, or posturo-dental, concept was developed in 1995 to highlight the primary role of dental occlusion in the overall postural balance of the individual.
With the posturo-occlusal concept, for the first time, dental occlusion was no longer examined and understood only in relation to dental contacts or in a dento-dental framework, but through the individual as a whole.
This global vision, proposed as early as 1989, was largely ignored by the dental community, as it clashed with the academic consensus and challenged received ideas.
It was not accepted any better by the posturological world, which at best did not understand the relationship between posture and dental occlusion and at worst saw a new player who was disturbing this already very complex discipline.
Dental problems may be the cause of your posture problems.
Objective of dental posturology
Traditionally, posturology is the study of the standing man through his three main sensors: the eye, the vestibule and the foot.
For us, posturology is above all a common, unified and multidisciplinary framework in which different health professionals will intervene: doctors, ENT specialists, ophthalmologists, podiatrists, rehabilitation specialists and dentists.
Posturology has provided rules and standards that have made the clinical examination more rigorous and objective. It has made it possible to objectify morphostatic modifications of patients during malocclusions and occlusion modifications.
Our approach thus has a double objective :
- To demonstrate the role of occlusion in posture
- To diagnose occlusal pathologies in postural deficits

1. The cranial concept of posture
The bipedalism and verticality that characterise hominisation are the result of a slow phylogenetic and ontogenetic evolution. Standing man is the result of a cerebral evolution, of a cerebral function. The spherical cranial shape corresponding to an orthognathic cranio-mandibular relationship appears to be a criterion of optimal verticality. At the same time, the ocular sensor becomes the main postural referential in humans in addition to the inner ear, the feet and the skin.
Similarly, our immersion and communication in the world is now more visual than olfactory, auditory or tactile. These facts have led us to propose a cranial concept of posture (1). For us, posture can be summed up as a head stabilised in space in relation to the visual axis, the axis of the gaze.
The eye provides the reference frame necessary for the execution of the movement; skiers and riders have surely already experienced this (5). This postural strategy of stabilising the head is almost constant throughout an individual’s life. The work of Amblard and Assaiante confirms that only children up to the age of 6 years use a strategy of stabilising the trunk in space.
What is remarkable and extraordinary for dentists is that the visual or labyrinthine plane is the Frankfurt plane. This means that there can be no occlusion without a postural reference to the Frankfurt plane, since the teeth belong to the skull.
The facebow and the articulator set-up are fully justified here. From this head, musculoaponeurotic postural chains ensure the stability of the standing man.
These chains were described by G. Struyf-Denys and then taken up by B. Darraillans and M. Clauzade in 1989.
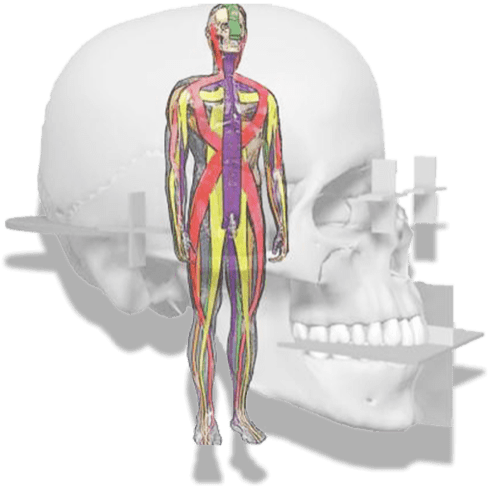
There are 5 musculoaponeurotic postural chains:
- 3 phasic anteroposterior chains called lingual, facial and central which ensure the anteroposterior balance of the individual. The mandible plays a regulating role.
- 2 tonic-phasic lateral chains called masticatory which ensure a relational function of introversion or extraversion.
2. The craniomandibular relationship
It constitutes the musculoskeletal and neuronal reference frame in which the dental occlusion takes place. This is in agreement with the theses defended by gnathologists, but also closer to us like R. Slavicek or Ph. Dupas.
It is necessary to distinguish between the box and the teeth: it is necessary to orient the box before placing the teeth.
2.1- In the antero-posterior direction
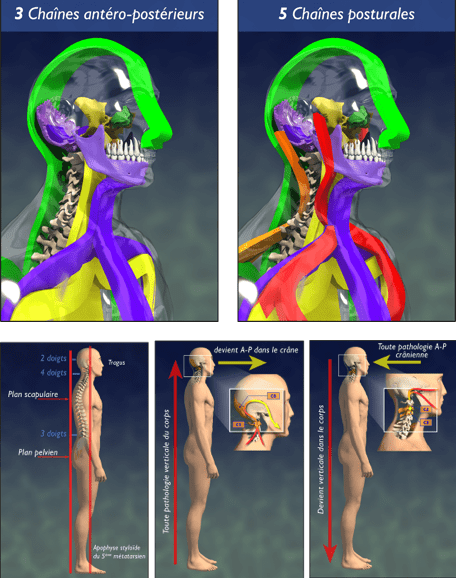
Anteroposterior postural organisation is subject to an orthopaedic law of compensation:
- Any cranial anteroposterior pathology or dysmorphosis will find a vertical postural compensation in the body.
- Any vertical postural pathology in the body will find an antero-posterior compensation in the skull.
The mandible thus plays the role of anteroposterior postural compensator, but also behavioural by regulating the anterior and posterior postural chains, i.e. lingual and facial.
2.2- Dans le sens transversal
Curiously, the human system does not have a buffer system, a transverse compensation system.
Any transverse dysmorphosis or dysfunction will be pathological and will result in a decompensation biotype. Crossbites or mandibular latero-deviations will necessarily induce a postural asymmetry and must be systematically treated.
However, the lesion may appear to be asymptomatic in the oral cavity and be exercised at a distance. It will then give rise to cervical pain, or even tendonitis or pubalgia.
In this transversal sense, we must include emotional or relational etiologies which are considered as transversal pathologies and which can then constitute systemic cofactors and thus tip a compensated system into a decompensated system.
In this systemic concept of pathologies, malocclusion must be considered as a necessary but not sufficient condition. The state of the system, its historicity, then provides the dynamics for the pathology.
Thus, two opposite dynamics can be conceived for the same class II/2 system:
- An asymptomatic functioning in an individual who presents a rich and gratifying social, affective and professional life.
- Dysfunction in an individual with multiple emotional, affective or social problems.
3. The temporomandibular joint
The temporomandibular joint (TMJ) is a region that fundamentally compensates between the two major postural systems that we will discuss later: the cranio-sacral system and the cranio-mandibular system. This region must be endowed with a particular nature and properties that allow it to assume this role.
A joint only plays a sliding or transmission role, there is no idea of remodelling or compensation. When it exceeds its adaptive capacities – either through trauma or excess – it breaks or tears.
This very particular specification has led us to qualify the temporomandibular joint as a “suture” in accordance with the work of P-H CAIX (17), G COULY (18-19), and J DELAIRE (20). This is a specialised cranial suture whose nature is confirmed by several facts:
- histologically, a suture is the joint formed between two mesenchymal bones. The squamosal of the temporal and the dental are mesenchymal in nature.
- In the 8th week of intrauterine life, cracks called “blasts” appear in the connective tissue between these two bones and give rise to the meniscus apparatus. It is therefore a contributed entity and not a unitary process as for a classical joint.
- at birth, the glenoid cavity is flat. It will take its adult convex shape under the action of mastication. Between birth and the age of 6 years, the TMJs undergo a positional drift and pass from an exo-temporal position to a sub-basi-temporal position.
- the presence of a particular cartilage, called “fibrocartilage”, in the glenoid cavity and the condyle, which has healing and remodelling properties.
This sutural state gives the mandible a permanent compensatory role and confirms the orthopaedic role we attribute to it. It formally contraindicates any surgical action that would have the consequence of transforming this sutural tissue into fibrosic tissue capable of creating post-therapeutic ankylosis.
4. The trigeminal
The dental surgeon does not work on teeth, but on the trigeminal system.
In this respect, his work is closer to that of a neurologist than to that of a mechanistic prosthodontist, to which he is confined. The nature of occlusion is essentially neurological and trigeminal. The trigeminal nerve is the nerve of the first branchial arch which will give rise to the face. Thus, the trigeminal is the neuro-matrix of the face.
4.1 The trigeminal and dura mater
The trigeminal is often apprehended in our profession only in its extra-cranial portion and its terminal branches V1, V2 and V3. However, these different branches present, before or after their cranial exit, meningeal branches which were described by LAZORTHES.
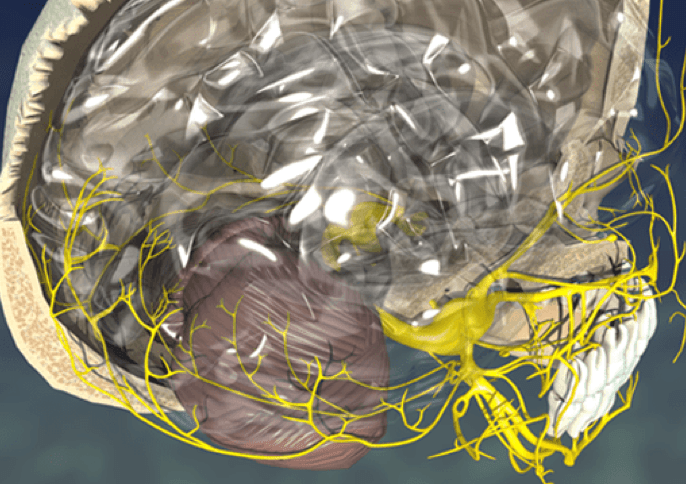
This trigeminal innervation of the dura mater (tissue element that forms the meninges) is crucial to consider in the physiology of the balance of the cranial function.
Osteopaths call these dura materia “reciprocal tension membranes”, because they manage the cranial tensional balance in the antero-posterior plane, but also in the transverse plane.
It is through these meninges that the cerebrospinal fluid flows from the villi of the 3rd ventricle. The fluctuation of the cerebrospinal fluid is the basis of the dynamics of the cranio-sacral system of osteopaths.
4.2 The trigeminal and reticular formation
The control of cardiac, pulmonary, intestinal vital functions, as well as wakefulness and sleep, takes place in the brainstem in a region called the “reticular formation”, which is a neuronal associative region with specific functionality and a network of connections (30).
Monoamine nuclei such as the locus coeruleus and acetylcholine are essential for memory and attention. They also play an essential role in the regulation of wake and sleep cycles.


We have reported that the motor nucleus of the trigeminal area is confused with the locus coeruleus (monoamine nucleus with norepinephrine or noradrenaline) and we have already shown the close relationship between the trigeminal area and the reticular formation (31-32-13-2)
The close relationship between the trigeminal and the locus coeruleus supports several statements :
- The proximity of the different nuclei of the reticulate and those of the trigeminal suggests inter-reactions and perhaps also “buggs” at the origin of the varied symptomatology that can be encountered in these dysfunctions, which can range from taste modification to mood modification of the person.
- Let us not forget that the mouth is the organ that has evolved the most during phylogenesis. B. CYRULNICK speaks of the “bewitched mouth” because it has evolved from a prehension-defence function to a verbalisation-speech function (33).
- In the light of all this work, is the trigeminal not one of the main vectors of the emergence of consciousness?
Located in the archaic brain, the trigeminal also participates fully in the construction of the proto-self, which is the first unconscious self (30).
The oral cavity and orality are the building blocks of any individual; foundations on which the cognitive structure will be built.
We understand better the confusion of our patients in the context of cranio-mandibular dysfunctions which necessarily present a mechanical structural side, but also an emotional and psychological side. Their management can be very complex and requires multidisciplinary teams including psychologists and psychiatrists.